Eye Doctors and Optometrists in Bakersfield, CA

YOUR PARTNERS IN EYE CARE
At Li and Liao Optometry, we are your partners in eye care, committed to serving your eye health needs and giving you clear vision for the best quality of life. When you visit our offices, you’ll receive a comprehensive, guided patient experience that respects your valuable time.
We want to make sure you understand why each service and treatment you receive is important, and that you feel comfortable and confident in your care. That’s why we explain your care every step of the way and answer any questions you may have: If you have concerns, we’ll provide solutions.
We Are Focused on You

Learn from Our Doctors
Our doctors are passionate about educating our patients regarding their eye health. Click below to see a few short clips of our doctors showcasing their passion in action:
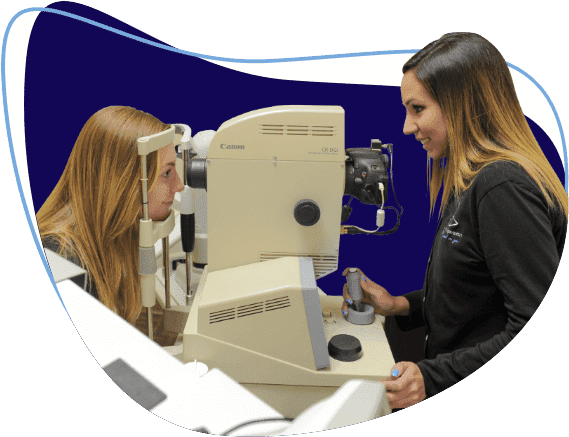
Our Team & Technology
To us, bringing you clear vision isn’t enough: you should have a comfortable experience whenever you’re with us, too, and that’s what our technicians help provide. At the start of your appointment, you’ll be assigned a technician to be an expert on you. They stay with you throughout your entire visit, listening to your needs and concerns and relaying them to our other staff so that everyone involved in your eye care is always on the same page.
Our eye doctors use advanced diagnostic technology to provide accurate scans and images of your eye, enabling us to diagnose any potential issues as early as possible. And to further aid them, our doctors have scribes on hand so they can focus on the smallest details and spend their time listening to you, not entering information into a computer.
Testimonials
Contact Us
We can't wait to serve you. Please fill out this form, and our team will be in touch to get you in as soon as possible.
Contact Us
"*" indicates required fields